April 23, 2024
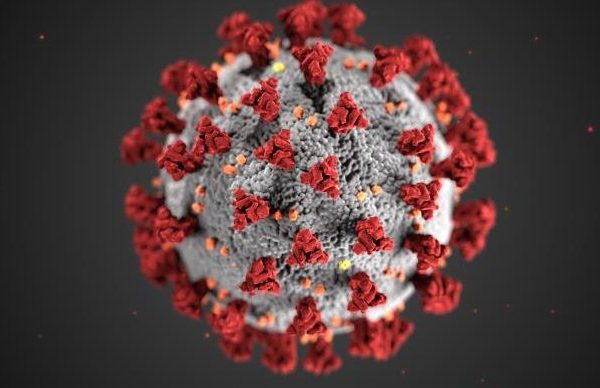
Coronavirus Updates
We are following the latest developments with COVID-19 and the recommendations by the Centers for Disease Control and Prevention.
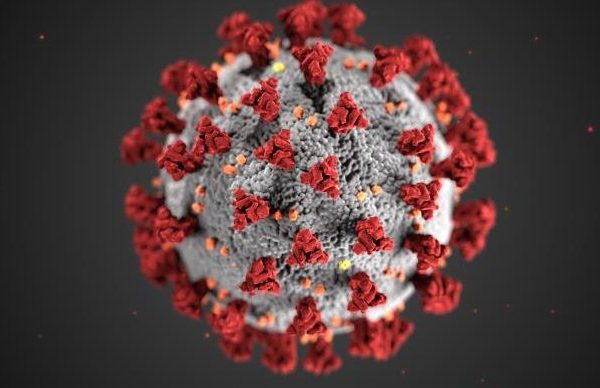
April 23, 2024
We are following the latest developments with COVID-19 and the recommendations by the Centers for Disease Control and Prevention.

April 23, 2024
UNC Lineberger hosted students from NCCU and NC A&T who were enrolled in an online course about career and academic opportunities in cancer care and research.

April 22, 2024
UNC Health oncologists and pathologist provide a basic overview of staging cancers and grading tumors, and why these categories are important to your medical team.

April 18, 2024
UNC Health radiation oncologist Ashley Weiner, MD, PhD, explains what radiation is and what you can expect if you’re preparing to receive treatment.

April 9, 2024
Lisa Carey, MD, ScM, FASCO, was honored for her distinguished service over the years leading outstanding clinical and translational research and her work in eradicating health disparities.

April 9, 2024
UNC Health social worker Rose Wilson, MSW, and UNC Health oncologist Jared Weiss, MD, discuss the physical and emotional considerations of long-term cancer care.

April 4, 2024
Kimberly Shoenbill, MD, PhD, MS, and Adam Goldstein, MD, MPH, outline the need for health professionals to work collaboratively to optimize tobacco cessation treatment in patients undergoing lung cancer screening.

March 26, 2024
Researchers and trainees from UNC and UNC Lineberger at will present more than 30 talks and participate in scientific and educational panels and discussions on the latest cancer research.

March 26, 2024
Your gift to UNC Lineberger provides resources for physicians and scientists to uncover the causes of cancer, to conduct groundbreaking laboratory research, and to translate findings into innovative clinical trials for treatments and cures.

March 21, 2024
Research by the lab of Jessica Thaxton, PhD, MsCR, and colleagues has unveiled new clues behind T-cell metabolism that could enhance immunotherapies that rely on T-cells to fight cancer.