UNC Lineberger researchers led by Cyrus Vaziri, PhD, describe the discovery of how a specific cellular protein present in cancer cells triggers a repair mechanism that allows them to DNA damage tolerance and abnormal growth.

Cancer cells can survive an attack by DNA-damaging drugs thanks to a protein that triggers a repair mechanism in the damaged cells, a University of North Carolina Lineberger Comprehensive Cancer Center research team has discovered.
In the journal Nature Communications, UNC Lineberger researchers describe how the protein helps to activate a pathway that allows cancer cells to copy their DNA even after sustaining damage to their genetic material.
They believe the findings could lead to new treatments that sensitize cancer cells to chemotherapy.
“We identified a new mechanism by which cancer cells resist DNA damage, including therapy-induced damage, by inappropriately activating an error-prone mode of DNA synthesis,” said the study’s senior author Cyrus Vaziri, PhD, a UNC Lineberger member and professor in the UNC School of Medicine Department of Pathology and Department of Biochemistry and Biophysics.
All cells must copy their DNA so that they can divide and grow. While damage to the DNA of normal cells can lead to their death, Vaziri explained that cancer cells can find ways to tolerate DNA damage and continue their growth – in some cases, even after anti-cancer drugs are used to deliberately damage cancer cells’ DNA.
Some anti-cancer drugs work by attaching big, bulky molecules to DNA that block DNA from replicating and stopping cell growth. Many cancer cells can find ways to work around blocks on DNA synthesis, Vaziri said, becoming treatment-resistant.
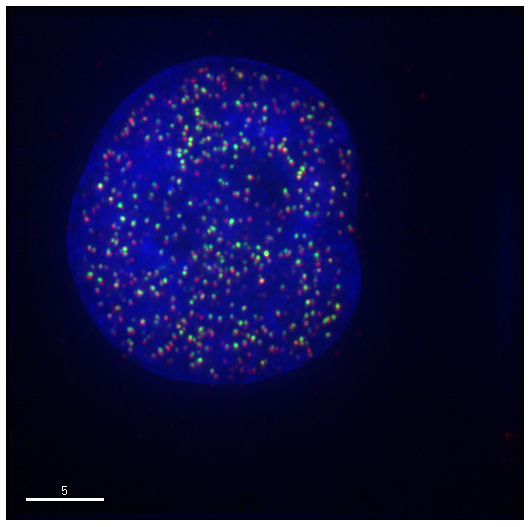
UNC Lineberger researchers have identified a way that cancer cells get around blocks to continue DNA replication. They discovered that cancer cells can activate “trans-lesion synthesis,” a molecular mechanism cells can use to duplicate DNA even when their genetic material is severely damaged. Vaziri said this process, known as TLS, is very sloppy and generates mutations in the DNA that can help continue to drive cancer.
The UNC Lineberger researchers found that many cancer cells express the MAGE-A4 protein to activate TLS. MAGE-A4 is normally found only in the testes, Vaziri said, but they found cancer cells hijacked the protein to jumpstart the TLS pathway to continue their DNA replication.
“We found the TLS pathway is inappropriately cranked up in cancer cells, and this does two things: It allows cancer cells to tolerate DNA damage, which allows them to avoid chemotherapy, and it gives them a way of increasing mutation rates,” Vaziri said. “This is significant because mutations drive cancer progression, and allow tumor cells to evolve and adapt to their environments.”
Study co-author Ben Major, PhD, a UNC Lineberger member and associate professor in the UNC Department of Cell Biology and Physiology, said the researchers used protein purification and mass spectrometry to identify the MAGE-A4 protein as a new member of the RAD18 protein complex. RAD18 is a well-studied activator of trans-lesion synthesis in cancer cells, thus supporting the connection between MAGE-A4 and TLS.
“The discovery of MAGE-A4s contribution to TLS is a novel finding that we expect will open the door to a drug discovery effort in the near future,” said Major.
The researchers believe that targeting this particular pathway could sensitize cancer cells to drugs that damage DNA. Very significantly, because MAGE-A4 is not found in most normal cells, agents directed against MAGE-A4 could be highly selective anti-cancer therapies. To test their hypothesis in future studies, the research team has developed a method to rapidly test small-molecule inhibitors of MAGE-A4, Vaziri said.
“Data from this study suggests that inhibiting MAGE-A4-induced TLS could combat chemoresistance by selectively making cancer cells more sensitive to chemotherapy,” said study co-author Ken Pearce, PhD, a research professor in the UNC Eshelman School of Pharmacy. “This has been a great collaborative effort between our labs and we all look forward to initiating the search for MAGE-A4-directed chemical probes and hopefully a novel therapeutic.”
In addition to Vaziri, Major and Pearce, the other authors include: Yanzhe Gao, Elizabeth Mutter-Rottmayer, Alicia M. Greenwalt, Dennis Goldfarb, Feng Yan, Yang Yang, Raquel C. Martinez-Chacin, and Satoshi Tateishi.
Individual researchers were supported by the National Institutes and by a Tier 1 Pilot Award from the University of North Carolina Lineberger Comprehensive Cancer Center.
