At the 10th Annual UNC Conference on Melanoma and Complex Skin Cancers: A Multidisciplinary Perspective, experts in melanoma treatment presented advances in treating the disease on Thursday. The conference, held at the William and Ida Friday Center for Continuing Education, drew dermatologists, surgeons, medical oncologists and other health care providers to hear presentations on topics ranging from immunotherapy drugs and targeted treatments for metastatic disease, radiation strategies, and chemotherapy to prevent skin cancer.
New treatments that unleash the body’s immune system against cancer or that target specific cancer-driving molecular pathways have expanded options for treating melanoma, the deadliest form of skin cancer.
At the 10th Annual UNC Conference on Melanoma and Complex Skin Cancers: A Multidisciplinary Perspective, experts in melanoma treatment presented advances in treating the disease on Thursday. The conference, held at the William and Ida Friday Center for Continuing Education, drew dermatologists, surgeons, medical oncologists and other health care providers to hear presentations on topics ranging from immunotherapy drugs and targeted treatments approved for metastatic disease, radiation strategies, and chemotherapy to prevent skin cancer.
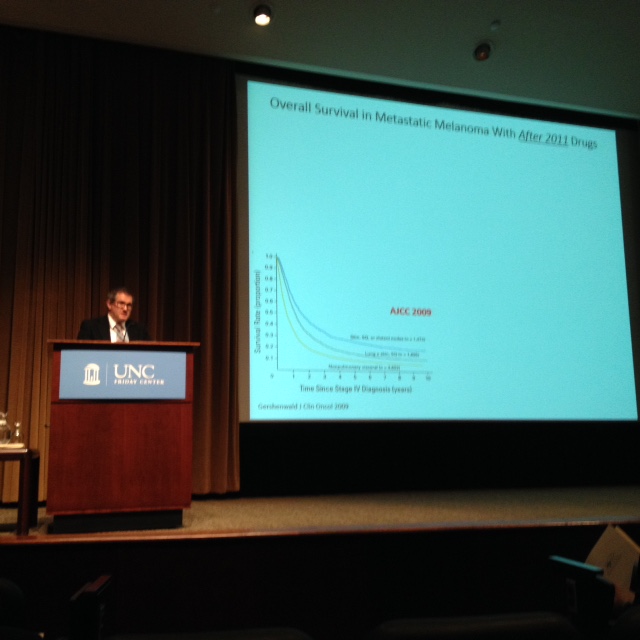
“With the approval of seven new drugs for advanced melanoma in the United States since 2011, we have options we haven’t had before to treat patients with this deadly form of skin cancer,” said David Ollila, MD, James and Jesse Millis Distinguished Professor of Surgery at the University of North Carolina School of Medicine, co-director of the UNC Breast Program, and a UNC Lineberger Comprehensive Cancer Center member. “This conference is about letting providers know about the new drugs, possible combinations and treatment options. But as much as we’d like to say we’ve made advances, we still had an estimated 10,000 deaths from melanoma last year. There’s still a long way to go.”
Patrick Hwu, MD, chair of the Department of Melanoma Medical Oncology at The University of Texas MD Anderson Cancer Center, delivered the H. Douglas Sessoms Memorial Melanoma Lecture. Hwu spoke on treatments recently approved by the U.S. Food and Drug Administration for metastatic melanoma, saying he’s more optimistic than he ever has been about treatment for patients with metastatic melanoma.
Hwu outlined two new areas of treatment for the disease in particular: targeted treatments, which are designed to response to particular mutations or molecular alterations in patients’ cancer, and immunotherapies, which unleash the body’s immune system against a patient’s own cancer.
The future of treating this disease, he said, is combining immunotherapies and targeted therapies together.
When the first targeted BRAF inhibitor treatments came out, Hwu said “it was a miracle,” and produced a Lazarus-type effect in patients. He described a bedridden patient who, after taking the drug, got up and took his kids to Disney World. While he said the future is to combine immunotherapy and targeted treatments, he outlined advisable ways to use them now. For example, he said targeted therapies like BRAF inhibitors should be used initially for patients with rapidly growing tumors, and then to switch to immunotherapy treatments once the cancer is under control.
A new immunotherapy treatment – the first “oncolytic” immunotherapy treatment — was just approved last year. Frances Collichio, MD, a UNC Lineberger member and clinical professor in the UNC School of Medicine Division of Hematology and Oncology, described her experience leading an arm of a trial at UNC for the new treatment, talimogene laherparepvec. The treatment uses a modified herpes virus to kill melanoma cells, and to draw the immune system to help fight the cancer as well. The drug is injected directly into the tumor, and because it is a viral treatment, it divides rapidly within the cell, and causes it to die. When the cancer cell dies, it releases proteins that attracts immune cells to the target area.
Collichio first heard of the then-investigational drug in 2007, at a time when there were few treatments available for patients with metastatic melanoma. The trial or talimogene laherparepvec started at UNC in 2009, and the last patient was enrolled in 2011. Collichio described administering the treatment, and watching dark-colored melanoma cells in the skin to shrink, change in color, and disappear While she said she hopes to see the drug administered in outpatient clinics, it can still require hospitalization. She emphasized that patients could come to melanoma centers of excellence for treatment of metastatic disease.
“There are so many treatments out there – if someone has just been diagnosed with advanced melanoma, go somewhere where they see a lot of this,” she said.
Bhisham Chera, MD, a UNC Lineberger member and an associate professor in the UNC School of Medicine Department of Radiation Oncology, spoke on a form of radiation treatment called radiosurgery, which involves using high doses of targeted radiation to treat skin cancer that has spread to the brain, limiting side effects. As opposed to whole brain radiation, radiosurgery limits side effects to the brain outside of the primary tumor, but is not as effective at treating micro metastatic disease.
UNC is pushing the envelope, Chera said, by combining immunotherapy drugs with radiosurgery to treat melanoma that’s spread to the brain. They believe that while the drugs don’t cross the blood-brain barrier, the infiltrating T-cells do increase in the brain.
“We’re going to back to look at our data and see if we have better control of the disease in the brain with these immunotherapy drugs and radiosurgery,” he said. “Going forward, I think the future in melanoma is how do we combine these newer systemic treatments with radiation to the brain to improve survival.”
Ollila co-directed the conference with Nancy Thomas, MD, PhD, a UNC Lineberger member and the Irene and Robert Alan Briggaman Distinguished Professor in the UNC School of Medicine Department of Dermatology.
