Transcription factors regulating blood oxygen linked to melanoma metastases
In an article published April 8 in the Journal of Clinical Investigation, a research team led by William Kim, MD, member of the UNC Lineberger Comprehensive Cancer Center, and graduate student and first author Sara Hanna, linked melanoma metastases to a pair of transcription factors known as HIF1 and HIF2.
Researchers found that HIF1 and HIF2 are overexpressed in melanoma tumors. In healthy cells, HIF1 and HIF2 assist in regulating hypoxia, the state caused by low levels of oxygen in the blood. Hypoxia has been linked to metastases in several solid tumors, and the UNC team has found that it promotes the spread of melanoma from the skin to other sites in the body through the lymphatic system.
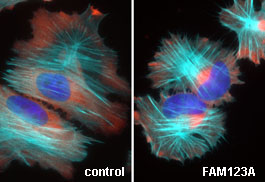
Patients who are diagnosed with early stage melanomas have a high rate of survival, but the prognosis worsens significantly once the tumors spread to other sites throughout the body. Using in vitro systems and mouse models, researchers suppressed the expression of HIF1 and HIF2 in the melanoma tumors. While the inactivation of the transcription factors did not reduce the growth of the initial tumors, it did reduce the rate at which the melanoma spread to other sites in the body.
Both HIF1 and HIF2 independently activate the protein kinase SRC using different signaling pathways. The SRC protein has been linked to several different cancers, and the identification of its role in melanoma suggests that existing therapies targeting SRC may prove to be a viable target for therapies aimed at reducing the spread and ultimate lethality of the cancer.
“What we are trying to do now is inhibit these pathways with drugs in the mice to see if we see a decrease of metastasis,” said Hanna.
UNC researchers who contributed to this article include Bhavani Krishnan, PhD; Sean Bailey; Stergios Moschos, MD; Pei-Fen Kuan, PhD; Marni Siegel and C. Ryan Miller, MD, PhD, of the Lineberger Cancer Center; and Lukas Osborne, E. Tim O’Brien III and Richard Superfine, PhD, of the UNC Department of Physics and Astronomy.
This research was supported by the National Institutes of Health (P30-DK-034987), the National Cancer Institute (3P30CA016086), the Department of Defense (W81XWH-09-2-0042) and the University Cancer Research Fund.
Date: April 19, 2013
