UNC Immunotherapy T32 Training Grant

Program Overview
The UNC-Chapel Hill Immunotherapy T32 Training Grant (IM-TAG) at UNC Lineberger Comprehensive Cancer Center is funded by a National Cancer Institute T32 training grant.
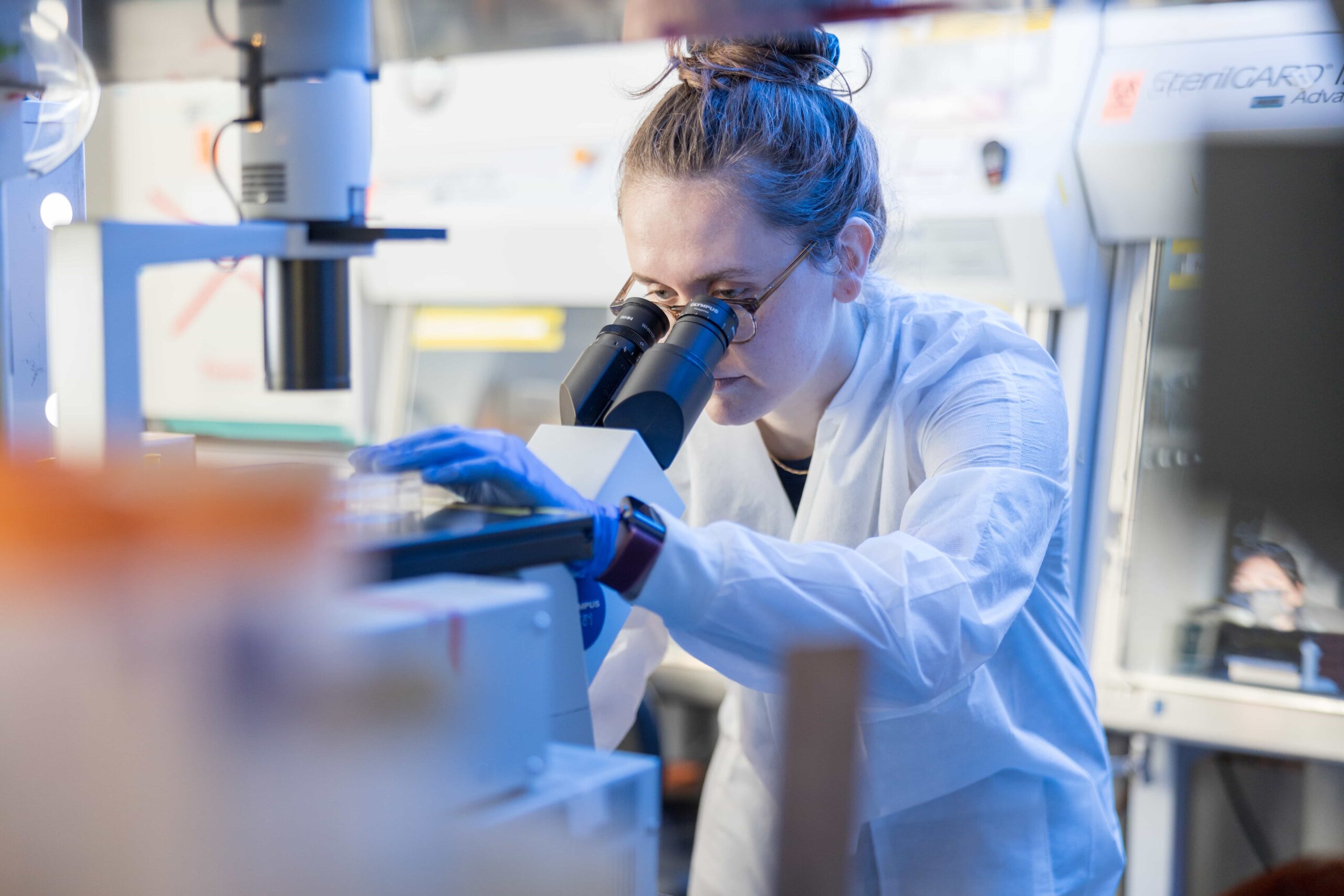
The program trains postdoctoral fellows in pre-clinical and/or clinical research focusing on tumor immunotherapy and/or stem cell transplantation immunology.
All UNC Lineberger postdoctoral researchers and clinicians interested in this area are eligible to apply. External candidates may also apply.
Program Leadership

Program Director
Jonathan Serody, MD
Elizabeth Thomas Professor of Medicine, Microbiology and Immunology
Associate Director for Translational Science, UNC Lineberger Comprehensive Cancer Center
Director, Cellular Therapy Program

Co-Program Director
Barbara Savoldo, MD, PhD
Champ Mitchell Professor of Pediatrics
Division of Pediatric Oncology
Co-Director, UNC Lineberger Comprehensive Cancer Center Immunotherapy Program
 Co-Program Director
Co-Program Director
Benjamin Vincent, MD
Associate Professor of Medicine, Microbiology and Immunology
Member Program in Computational Medicine
