UNC Lineberger member James Bear, PhD, uncovers the intricate mechanisms that allow certain cells to move, discoveries with implications for cancer metastasis.
By Mark Derewicz
What if cancer cells couldn’t move? What if patients – once they’re diagnosed with cancer – could take a drug that made cancer cells immobile? The answer is simple: survival rates would skyrocket. But reality is complicated. It’s hard to know with precision how metastasis happens. But that’s what James Bear, PhD, professor of cell biology and physiology, is trying to do – understand cell movement so he and others can do something about it.
“We don’t normally think of cells moving around, but they actually move around all the time,” Bear said. “It’s called cell migration. It’s natural.”
The problem is when cancer cells move, eradicating them becomes nearly impossible. This is the so-called stage 4 cancer – when cancer cells in one organ take up residence in several other parts of the body. Bear’s lab at the UNC Lineberger Comprehensive Cancer Center is unraveling the mysteries of cell migration one tiny cellular mechanism at a time. Much of the time his team works with healthy cells. Turns out, even understanding how normal cells migrate is no easy task.
And, as Bear can attest, sometimes a seemingly simple experiment turns into a three-year experimental odyssey of trying to understand how even common, healthy cells such as fibroblasts move.
Back to Basics
So, how do they move?
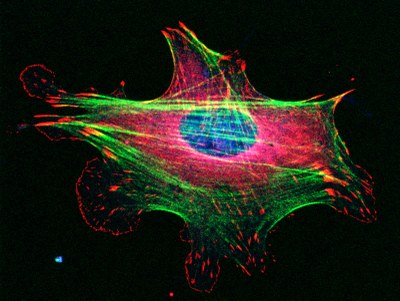
Big picture: cells move thanks to their cytoskeletons – miniature, internal skeletons composed of filaments, which are made up of proteins. How those proteins work and interact with each other and their environments is, well, part of a smaller, more complicated picture.
One of the “protein-filament” systems Bear studies is the actin cytoskeleton. Actin was originally discovered as one of the main muscle proteins. It helps muscles contract. But actin is in every cell in the body. In non-muscle cells, actin is one of the driving forces behind cell migration. The actin cytoskeleton is torn apart and rebuilt over and over on a sub-second timescale to allow the cells to move. Each time a cell rebuilds the actin filaments, tiny proteins must glue these filaments together in specific architectures so the cell can move over a gradient – up an incline or across a substance in the body.

“It’s like building a skyscraper, tearing it down, and building another right next to it,” Bear said. “The filaments are like the iron beams that must be attached with rivets at specific angles.”
It’s just that, with cells, the rivets are binding proteins that not only attach the filaments together at specific angles, but must do so in a way that allows the cells to move. One of the main binders is a protein complex called Arp2/3.
“For a long time, scientists thought that you couldn’t study Arp2/3 in a lab because as soon as you manipulated it, the cell would die,” Bear said.
But in 2012, Bear’s lab managed to manipulate Arp2/3 in fibroblasts. In fact, his lab was the first to generate a viable cell line without Arp2/3. This allowed his team to study the precise role of this protein complex in cell movement that depended on cues in the cells’ environment. That’s crucial because all cells move in specific ways and certain directions depending on cues in their surroundings.
“It’s like when you drive a car; you’re guided by visual cues,” Bear said. “Cells need signposts. There are chemical cues that serve as signposts that allow for directed migration.” Directed, as opposed to scattershot. Cells, such as fibroblasts, have purposes. To help heal a wound, for instance, cells need cues to get where they need to be.
This directed movement is called chemotaxis.
“We assumed that fibroblasts would not be able to chemotax without the Arp2/3 complex,” Bear said.
So he set up a basic control experiment to prove it. His team used a technology called microfluidics to create a tiny chamber wherein cells could move and Bear’s team could study the movement over time – an experiment that had been difficult to accomplish with previous technologies.
Bear found that not only could cells survive without the complex, but that fibroblasts were able to slowly crawl in the right direction up a gradient of a chemical cue. “We were very surprised,” Bear said. “We did the experiment again and again and again, and each time the cells could chemotax. Essentially, the three years that followed were a control experiment run amok.”
Bear knew that the cell’s basic machinery of motility was messed up. Yet, the cells chugged up the gradient anyway, though 5 times slower than usual. Interestingly, the cells lacking Arp2/3 could not pick up a different directional cue – the extracellular matrix over which they crawled – indicating that Arp2/3 is important for some kinds of directional migration, just not chemotaxis. These results were published in 2012 in the journal Cell.
Bear thought, “Well, what do fibroblasts need in order to move up the gradient?”
This question began a series of complex, frustrating experiments that eventually led to a culprit. And it’s one that could very well be important in diseases that involve fibroblast-like cells – fibrosis, for instance, which is a chronic obstructive pulmonary disease, a very serious condition of the lungs.
Science, interrupted
One reason fibroblasts are a good cell to study, when it comes to chemotaxis, is that we very much need them to move during wound healing. In an infected wound, macrophages are the front line of the body’s immune response, wiping out infection and clearing away damaged tissue. But over the course of weeks and months, fibroblasts surround the wound to reorder the tissue so that it is properly repaired. Also, fibroblasts are part of the overactive immune response in COPD; they contribute to the narrowing of the airway, which causes breathing difficulties.
“Fibroblasts clearly migrate according to directed cues,” Bear said. “And we know one of the main cues – platelet-derived growth factor, or PDGF.”
So Bear’s team set out to find the precise cellular pathways used in chemotaxic response to PDGF, pathways that could one day become a therapeutic target.
Bear knew that fibroblasts have a cell receptor called PDGF-R. He thought that blocking the ability of PDGF to latch onto the receptor should stop the cells in their tracks. And it did.
“This showed us that we could block chemotaxis if we blocked all the cell-signaling pathways downstream of PDGF,” Bear said. “So we wanted to check those pathways downstream of PDGF to find out the specific ones that were causing this response.”
The first two pathways they checked – called PI3 Kinase and TOR – had been implicated in chemotaxis of amoeboid cells, which traditionally have been much easier to study than fibroblasts. In fibroblasts, though, Bear found that PI3K and TOR didn’t do anything to stop cells from moving. “That was a big surprise,” he said. “So, again, we realized that something else had to be going on.”
Then, with help from the lab of Ned Sharpless, MD, the director of Lineberger, Bear’s team developed two melanoma cell lines with actin fibers arranged in the same way as fibroblasts. They had stress fibers and adhesions, like fibroblasts. They also had severe defects in two signaling pathways that were supposed to block chemotaxis.
Again, no dice. The cells could still move in a directed fashion in spite of the defects.
“At this point, we were really getting frustrated,” Bear said. “We thought, okay – just generally – what do cells absolutely need in order to chemotax. Well, for a cell to move, force has to be generated. And for a cell to move in a directional way, the force has to be asymmetrical – the force has to be aligned to an external cue, a gradient.”
Bear wondered which molecule generates force? He thought of myosin, which is famous for its important role as a motor protein in muscle. But like actin, it is also in other cells. It binds to actin and essentially walks along the actin filaments when cells move.
In amoeboid cells, myosin is in the back of cells. It squeezes the contents of a cell forward, sort of like toothpaste up through a tube. In fibroblasts, though, myosin is scattered throughout the cells. So Bear knew myosin likely worked differently in these cells.
Sure enough, when he applied a chemical inhibitor of myosin, the cells could migrate at a decent speed but they did so randomly; they were no longer capable of responding to a directional cue in their environment. Then Bear’s team washed out the inhibitor, reset the PDGF gradient again, and the cells immediately moved up the gradient as they normally would.
“So, finally, we figured out that we need myosin for the cells to pick up the directional cue from PDGF,” Bear said. “We then decided to do a genetic experiment to knockdown the two major myosin isoforms [varieties of the myosin protein] that our inhibitory drug targeted.”
When Bear’s team knocked out myosin IIB, the cells could still chemotax. Without myosin IIA, however, the cells couldn’t move at all.
Through a series of experiments with Bear’s new microfluidic chamber system, his team sussed out the various proteins and events that regulate myosin-A. Down at the bottom of this long, three-year rabbit hole, Bear found something that fibroblasts absolutely need in order to move up a gradient – protein kinase C that acts to locally inhibit myosin IIA, which creates that “up through the toothpaste” kind of asymmetry in force that pushes cells along. According Bear’s research, it is the only thing that cannot be rescued through some alternative means to restore chemotaxis. These findings were published in 2014 in the journalDevelopmental Cell.
So, what does this mean?
“Our work suggests that we need to rethink how cells migrate toward directional cues,” Bear said. “I can’t say whether interfering with chemotaxis will affect COPD, but it might, because these fibroblasts wind up piling into the lungs, liver, and kidneys over time in people with this disease. If we could keep those cells out of where they’re not supposed to go, then that would be a good thing.”
Also, now that Bear’s team has mapped out this cellular pathway important for cell movement, it provides scientists with another piece of the metastasis puzzle.
“More than anything, though, these experiments revealed a really interesting piece of our underlying biology,” Bear said. “I think fibroblasts are like the utility infielders of the body; they do all kinds of jobs and they’ve clearly been underappreciated.”
Because many cells adopt similar attributes to fibroblasts, Bear’s work detailing the intricate interplay between cellular proteins, events, and structures during chemotaxis provides a model for never-before understood biology in one of the most mysterious but common events in human biology – cell migration.
“Will there be a drug in clinical trials next week because of this work? No.” Bear said. “But that’s not how science works. Basic science is about building our understanding from the ground up. We first need to know what happens in normal cells, in normal biology. Until we understand that, understanding what happens in a disease state won’t have any context.
“Frankly, we can give patients treatments and see how they work through trial and error, which is how a lot of medicine has worked, especially in the cancer field, for decades,” Bear added.
Some treatments have worked. A lot haven’t. Better therapeutic targets will only be uncovered through basic science.
“The real difference now as opposed to 20 years ago is we have better experimental tools and a better conceptual understanding of how cells work, and we think this will allow us to create ways to truly treat the underlying causes of diseases.”
The National Institutes of Health funded this research. Bear is an Early Career Scientist at the Howard Hughes Medical Institute.
Mark Derewicz is the science communications manager for the UNC School of Medicine.
