Significance
Over 80% of pediatric cancers occur in low- and middle-income countries (LMIC), where most health centers lack access to the key tools required for accurate diagnosis, disease classification, or appropriate treatment.
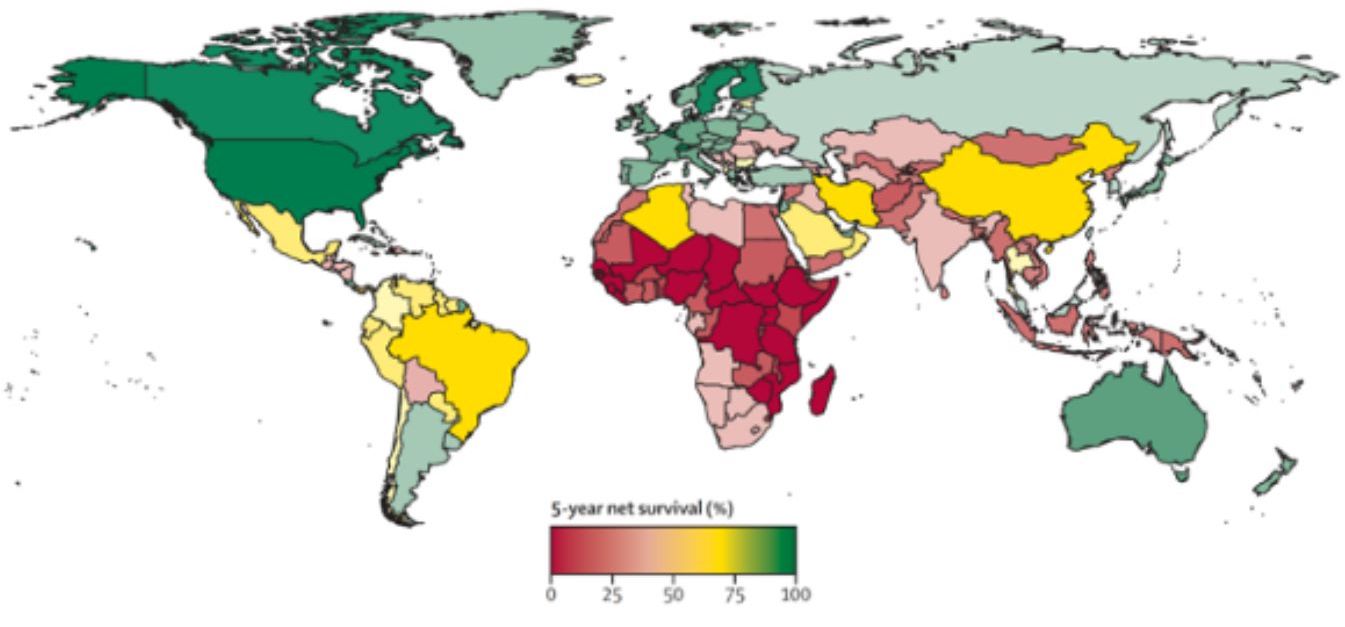
Consequently, although over 80% of children with cancer in HICs like the United States will survive, only 20% of children with cancer in LMICs will survive (Fig. 1). Worse yet, 50% of children who develop cancer in LMICs are never even diagnosed, meaning that they have a near 0% chance of surviving long-term. This “80/20 paradox” thus represents one of the largest health-related disparities in global health. Reframed, the most important prognostic factor for whether a child who develops cancer will survive is not related to cancer biology but is determined by where they live.
Deficiencies in several domains contribute to this survival disparity, including multi-level financial hardship, a trained and dedicated workforce, access to medications, and diagnostic testing.
A comprehensive clinical diagnosis of childhood cancers in HICs relies on multiple costly and time-consuming techniques such as immunohistochemistry (IHC), flow cytometry, cytogenetics, fluorescence in situ hybridization (FISH), targeted PCR panels, and microarrays. Most facilities in LMICs lack access to some or all these tests. Transformative diagnostic approaches utilizing cost-effective, rapidly scalable, and flexible technology are urgently needed for pediatric oncology if the global community is to meet the Global Initiative for Childhood Cancer targets by 2030.
In 2018, to raise awareness and improve outcomes for children with cancer in LMICs, the World Health Organization (WHO), together with other stakeholders, announced the Global Initiative for Childhood Cancer. Placing childhood cancers as a major global priority for the WHO, the Global Initiative for Childhood Cancer has set an ambitious goal of improving survival to >60% for all childhood cancers by 2030.
To achieve this goal, improving access to essential diagnostics and accurate treatment is imperative, which is the focus of UNC RAISE. In close collaboration with St. Jude Children’s Research Hospital and many international collaborators, our multidisciplinary team is advancing the development and implementation of sequencing-based diagnostics across domains of implementation science frameworks, health economics, bioethics, and technical / computational progress,