What does a year look like for the UNC Lineberger Comprehensive Cancer Center?
It’s exciting discoveries and cutting-edge research that bring new cancer treatments to our clinics. It’s compassionate and personalized patient care. It’s the many inspiring stories of strength, innovation, curiosity and hope lived by our patients and their families, and our physicians, researchers and staff.
As we prepare to enter a new year, we look forward to telling many more stories of hope and healing. We look forward to sharing the next big breakthrough in cancer research and treatment. And, most importantly, we look forward to growing and continuing to serve as a beacon of cancer care and research in North Carolina and beyond.
Join us as we reflect on stories from 2023 that inspired us throughout the year.
NIH and FDA award $18.6M to UNC Tobacco Center of Regulatory Science
The National Institutes of Health and the United States Food and Drug Administration awarded the University of North Carolina at Chapel Hill’s Tobacco Center for Regulatory Science (TCORS) $18.6 million to further research into tobacco product regulations.
UNC TCORS was launched at UNC Lineberger in 2013 and provides scientific studies that inform FDA’s regulatory authority for tobacco products. The center is led by Kurt Ribisl, PhD, program leader of cancer prevention and control at UNC Lineberger Comprehensive Cancer Center.
The integrated set of the center’s four current research projects seeks to understand the impact of regulations and communication campaigns on people who are disadvantaged by tobacco use disparities.

“Tobacco products cause 480,000 premature deaths in the United States each year. The results from our UNC research projects will inform current and future FDA regulations that will reduce the amount of death and disability caused by tobacco products.”
—Kurt Ribisl, PhD

N.C. Basnight Cancer Hospital opens Young Adult Outpatient Infusion Clinic
The Be Loud! Center for Young Adult Cancer Care was designed by former UNC cancer patients and is led by Lauren Lux, MSW, LCSW, and Andrew “Smitty” Smitherman, MD, at the UNC Adolescent and Young Adult Cancer Program in the UNC Lineberger Comprehensive Cancer Center.
The UNC AYA Cancer Program offers one-on-one support and counseling, AYA-specific resources, recommendations for clinical trials and treatment protocols, AYA survivorship care, care coordination and connection to other UNC cancer support services, programs and events for patients, and connections with other AYA individuals with cancer.

“The crux of the issue and why we built this space is that teenagers and young adults can get lost in the healthcare system. We wouldn’t be here without the phenomenal leadership at UNC Lineberger and UNC Hospitals. We know UNC believes in what we’re doing and supports the mission of the work. Everyone has been on the same page about how critical this mission is, and that is a huge gift to us.”
—Lauren Lux, MSW, LCSW
Two subtypes of HPV-associated head and neck cancers predict treatment outcomes
New research shows that HPV-positive head and neck cancers can be divided into two distinct subtypes that determine how well patients will respond to therapy, with one subtype being more responsive to radiation therapy.
Currently, many patients with head and neck squamous cell carcinoma are treated with high doses of radiation combined with chemotherapy. But the side effects – which include muscle fibrosis, swallowing difficulties, and artery hardening – can last a lifetime. Personalized therapy may allow oncologists to make better treatment choices for their patients; however, it can be difficult for doctors to determine the type and intensity of treatment without knowing how the patient’s tumor will respond to therapy.
Much to their surprise, Travis Schrank, MD, PhD, Natalia Isaeva, PhD, Wendell Yarbrough, MD, MMHC, FACS, and colleagues found the two distinct subtypes directly correlated with patient outcomes. Ultimately, this data could be used to identify patients whose therapy can be safely de-intensified in order to treat the tumor, lessen side effects, and enhance quality of life.
Now that researchers have more of an understanding of the new mechanism of HPV carcinogenesis, the findings may lead to the development of new, personalized treatments that are more efficient and have fewer side effects.
“We’re the first ones to describe these two subtypes. Using this research, we can firmly identify two groups of patients and are able to associate their tumor subtype with treatment outcomes.”
—Wendell Yarbrough, MD, MMHC, FACS

Parenting with cancer: New clinic helps parents navigate tough issues
Parents who receive a cancer diagnosis not only have to battle a serious disease — they also grapple with how best to talk to their kids about their illness, continuing to be there for them as much as possible, making sure their legal and financial affairs are in order, and other challenges.
The newly established Parenting with Cancer Clinic can help parents with cancer navigate those questions and get the help and support they need. Justin Yopp, PhD, a clinical psychologist who specializes in providing therapeutic services for families facing cancer, leads the clinic with Cindy Rogers, JD, an attorney who uses her legal expertise and network to guide patients and families to the right resources.

“Generally, almost every parent thinks about two key issues: how are my kids doing, and how will they be in the future? Parents with cancer have the same questions. These conversations are about securing their children’s current and future wellbeing. These can be hard conversations, so we want to meet each patient where they are.”
—Justin Yopp, PhD
Immune system B-cells can help predict HER2-positive breast cancer treatment response
Understanding why cancers respond, or don’t respond, to therapy is crucial to effective and personalized treatment.
Lisa A. Carey, MD, ScM, FASCO, Charles M. Perou, PhD, Aranzazu Fernandez-Martinez, MD, PhD, and colleagues found that measuring activation of immune system B-cells may be better than measuring either T-cell activation or the total number of immune cells in and around a tumor in predicting whether HER2-positive breast cancer responds to treatment.
In HER2-positive breast cancer, the immune system is key to the effectiveness of response to anti-HER2 drugs. Important cells in the body’s immune system include B-cells, which create antibodies that neutralize cancer cells and infections as well as T-cells, which directly fight cancers and infections.
“When there are active immune cells circulating around a tumor, the cancer tends to be easier to treat and cure. This is important because determining immune cell activity may allow us to identify which women with HER2-positive breast cancer will do well with standard, or even minimized, therapy.”
—Lisa Carey, MD, ScM, FASCO

UNC Lineberger hosts White House Chief Science & Technology Advisor
White House staff reached out to UNC Lineberger leadership to arrange a visit from the President’s Chief Science and Technology Advisor Arati Prabhakar, MS, PhD, who met with leading UNC Lineberger researchers to discuss their work supported by the Cancer Moonshot program and other innovative research in improving cancer prevention.
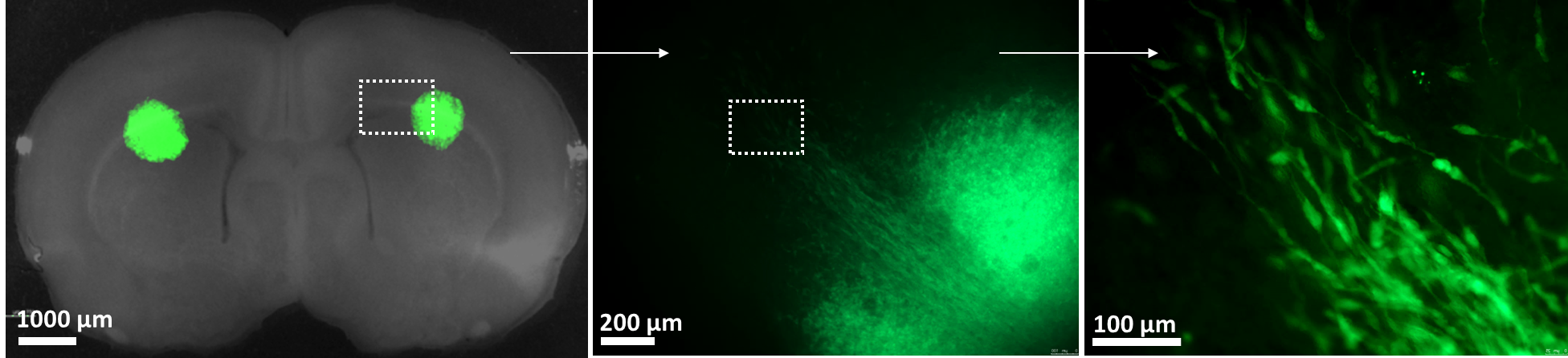
Devising a smarter way to treat brain tumors
Aggressive brain tumors are notoriously tough to treat. Many tumors are difficult to reach because they grow deep into the brain.
The protective capillary system surrounding the brain can weaken a drug’s ability to kill the tumor cells it’s meant to target. And the complexity of different brain tumor mutations can render some genetic analyses ineffective. These and other factors can make it a challenge for patients and their doctors to decide on the best course of action.
UNC Lineberger scientists have developed a tool called a “slice platform” that may help make those decisions easier. Running point on the innovative project is Andrew Satterlee, PhD, who has a powerful personal incentive to advance this technology: as a 20-year-old college student, he was diagnosed with brain cancer. The surgery to remove the cancer was successful, but because his tumor was rare, his doctors could not agree on what kind of chemotherapy regimen would best prevent recurrence. The decision was left with Satterlee and his family, who did a lot of research themselves and consulted with outside experts for advice and guidance.

“I feel so lucky to be developing this tool because I know how helpful it can be. If this test can offer an objective data point and ease the burden on patients, it can be a really important puzzle piece to help physicians make care decisions.”
—Andrew Satterlee, PhD

Cervical cancer screening doubles when under-screened women are mailed testing kits
Jennifer Smith, PhD, MPH, Noel Brewer, PhD, and colleagues found that mailing HPV self-collection tests and offering assistance to book in-clinic screening appointments to under-screened, low-income women improved cervical cancer screening nearly two-fold compared to scheduling assistance alone.
An estimated 14,000 women will be diagnosed with cervical cancer in the United States this year, according to the National Cancer Institute, and the cancer will lead to more than 4,300 deaths. Cervical cancer disproportionately affects Black and Hispanic women, with Hispanic women having the highest incidence rates, and Black women having the highest mortality rates for the disease in North Carolina and in the United States. Most cervical cancers occur among under-screened women.

“We’re now working with clinical partners to identify women who might be overdue for screening through electronic medical records. We hope to provide the option of either mailing them a self-collection kit to use at-home to mail back to us or hand a kit directly to them when they come into clinics for other services with the vision to eventually make self-collection a regular clinical provision.”
—Jennifer Smith, PhD
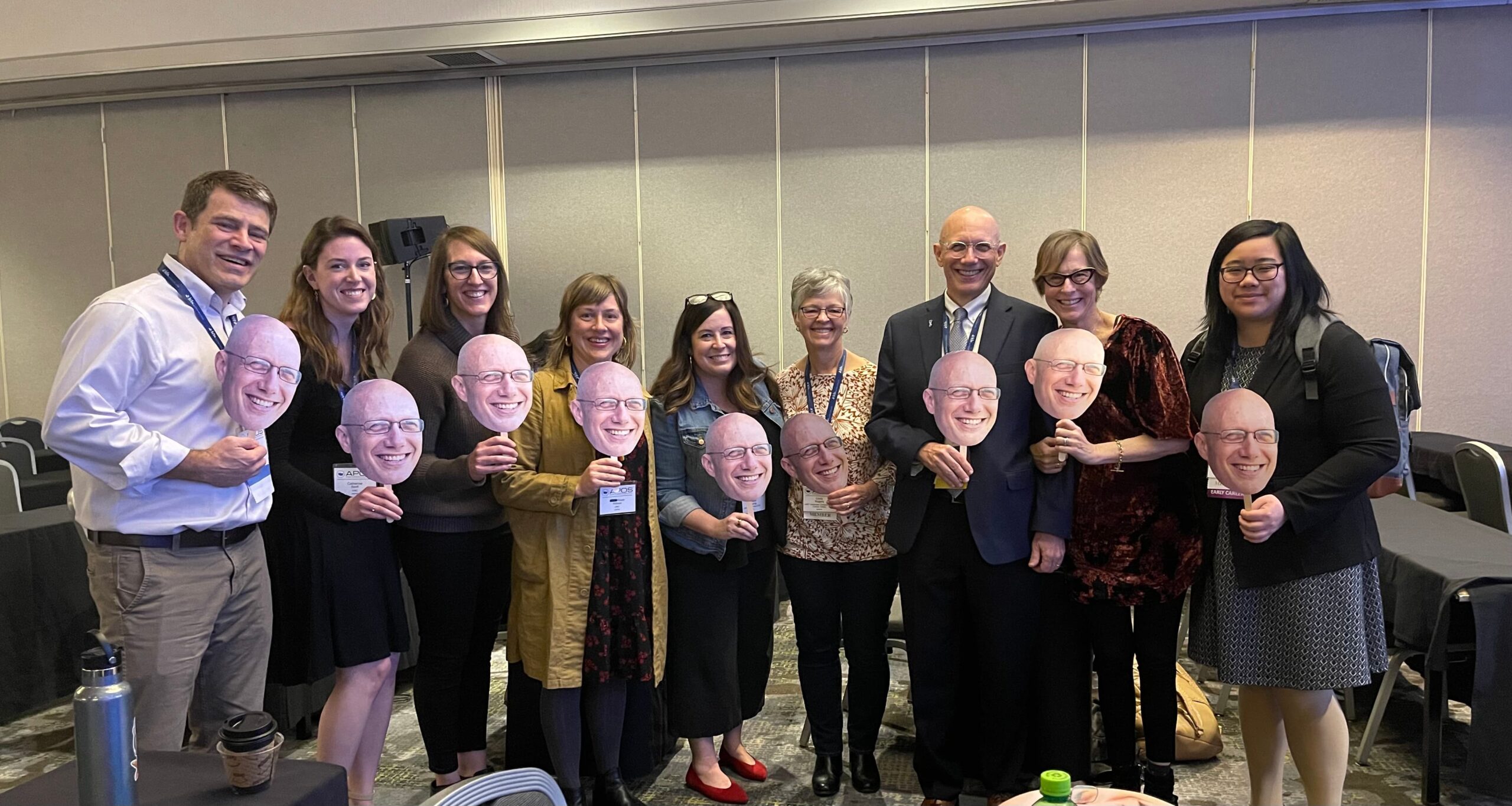
American Psychosocial Oncology Society honors Rosenstein with lifetime achievement award
The American Psychosocial Oncology Society (APOS) presented UNC Lineberger’s Donald Rosenstein, MD, with the Jimmie Holland Lifetime Achievement Award during its 20th annual conference. The awardee is recognized for distinguished leadership in the field of psychosocial oncology, with outstanding contributions in leadership, training, research, clinical practice, and service to APOS.
Rosenstein, a professor of psychiatry and medicine at the University of North Carolina School of Medicine, is the founding director of the Comprehensive Cancer Support Program at the N.C. Basnight Cancer Hospital, UNC Lineberger’s clinical home, and division head of general adult psychiatry in the department of psychiatry.
“Don is one of the most respected leaders in the field of psycho-oncology and we were so fortunate he accepted our offer to join our faculty in 2009 as we opened the N.C. Basnight Cancer Hospital. We wanted a visionary leader to establish our comprehensive cancer support program for all who came to us for care. His blend of innovation, humanity, and practicality led us in a spectacular fashion, from new ideas to improve the well-being not only of the patient but the family to growing a program that has quadrupled in size.”
— UNC Lineberger Director Shelley Earp, MD

Study provides guidance on quality-of-life choices for rectal cancer treatments
A multi-institutional study designed to compare two treatment options for locally advanced rectal cancer while collecting patient-reported treatment side-effects has generated insights patients can use to make more informed quality-of-life treatment choices in consultation with their doctors.
Led by Ethan Basch, MD, MSc, the multi-institutional quality-of-life study is a component of PROSPECT, a large national, phase III clinical trial to evaluate whether patients receiving treatment for localized rectal cancer can receive chemotherapy alone instead of the current standard approach of radiation therapy with some chemotherapy prior to surgery.
The patient-reported quality-of-life outcomes provide essential information for patients to weigh between these treatment options.

“Patients ideally will understand the potential impact of treatments on how they feel and function when making choices, so as oncologists we need to talk with our patients about their options and the consequences of those options.”
—Ethan Basch, MD, MSc, FASCO

Earp to step down as director of UNC Lineberger Comprehensive Cancer Center
Shelton “Shelley” Earp, MD, announced his intention to step down as director of the UNC Lineberger Comprehensive Cancer Center, effective in June of 2024.
Earp has served as UNC Lineberger’s director since 2018. This is his second stint in the role, previously leading the institution from 1997-2014. A graduate of the UNC School of Medicine, Earp has been a member of the UNC School of Medicine faculty since 1977. He will continue in his role a Distinguished Professor of Cancer Research, Medicine, and Pharmacology.
Under his leadership, UNC Lineberger has become one of the nation’s leading cancer research hubs, connecting faculty from across the University and beyond.

“The UNC School of Medicine and UNC Health have benefited greatly from Shelley’s decades of leadership. He has helped bring world class clinician-scientists and researchers together to answer so many complex questions in the field of cancer research and treatment. Our mission is to improve the health and well-being of the people of North Carolina, and Shelley’s work has done that.”
—CEO of UNC Health and Dean of the UNC School of Medicine Wesley Burks, MD

