Cases of human papillomavirus-associated cancers of the head and neck, known as head and neck squamous cell carcinoma (HNSCC), are rapidly increasing throughout the United States. Unfortunately, relatively little is known about the factors that contribute to these tumors and what makes some tumors more aggressive and treatment-resistant than others.
To determine why some patients respond better to radiation therapy than others, researchers in UNC School of Medicine’s Department of Otolaryngology/Head and Neck Surgery and the Lineberger Comprehensive Cancer Center formed a robust collaboration with researchers at Yale Cancer Center, the Yale Head and Neck Cancer Specialized Program of Research Excellence and the ECOG-ACRIN Cancer Research Group (ECOG-ACRIN).
Together, they published a new study in Proceedings of the National Academy of Sciences, which reveals that HPV+ head and neck cancers can be divided into two distinct subtypes that determine how well patients will respond to therapy, with one subtype being more responsive to radiation therapy. Researchers also discovered a new mechanism of HPV carcinogenesis through the study which enhances growing efforts to personalize treatment for patients with HPV+ HNSCC.
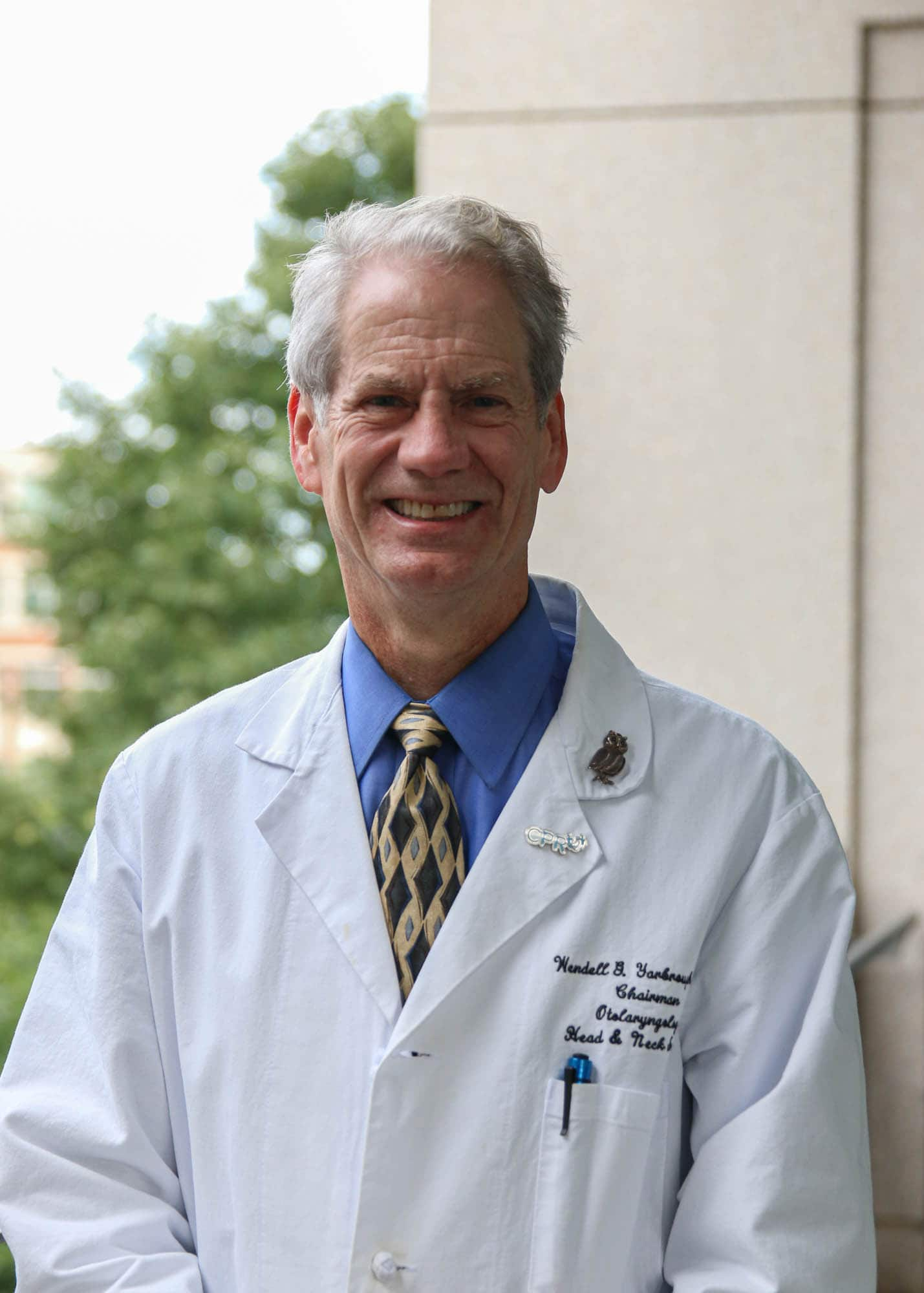
“We’re the first ones to describe these two subtypes,” said Wendell Yarbrough, MD, MMHC, FACS, the Thomas J. Dark Distinguished Professor of Otolaryngology/Head and Neck Surgery, “Using this research, we can firmly identify two groups of patients and are able to associate their tumor subtype with treatment outcomes.”
Currently, many patients with HPV+ HNSCC are treated with high doses of radiation combined with chemotherapy. But the side effects – which include muscle fibrosis, swallowing difficulties, and artery hardening – can last a lifetime. Personalized therapy may allow oncologists to make better treatment choices for their patients; however, it can be difficult for doctors to determine the type and intensity of treatment without knowing how the patient’s tumor will respond to therapy.

To address this need, members of Yarbrough’s team, including Travis Schrank, MD, PhD, Natalia Isaeva, PhD, and Wesley Stepp, MD, PhD, who were also co-authors on the paper, began coordinating a research cohort at UNC, grabbing publicly available data from the University of Chicago, and some validation data from E1308, a large national cooperative group clinical trial that was done through ECOG-ACRIN.

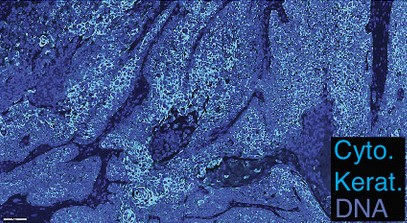
They then analyzed the tumor samples and identified several groups of co-expressed genes. Only one of these co-expressed gene sets separated tumors with high and low expression, and analysis of genes in this set found that they represented targets of a master transcription factor called NF-kB. NF-kB plays important roles in inflammation and cell death and has been associated with carcinogenesis of HNSCC.
Much to their surprise, researchers found the two distinct subtypes directly correlated with patient outcomes. Tumors with low NF-kB activity were associated with worse prognosis, while tumors with high NF-kB activity were associated with a better prognosis.
The subtypes identified by high or low NF-kB activity were remarkably different from one another, from the genes that were mutated in the cancers, factors driving the mutations, the number of mutations per cancer, HPV gene expression, HPV integration, gene methylation, and infiltration of certain immune cells into the tumor.
“One of our very tenacious, intelligent residents, Wesley Stepp, who is a co-author in the paper, was really instrumental in organizing that set of patients in the UNC cohort,” Schrank said. “All of the organizations that collaborated on this research project were very willing to work with us.”
Patient survival was the most obvious, and important, distinction between the two types of tumors. To get a better understanding of why one subtype may have better outcomes, researchers constructed cellular models of each subtype in the lab.
“Tumors with high NF-kB activity were more responsive to radiation therapy potentially contributing to improved patient survival,” Yarbrough said. “We know that there’s something about activating the NF-kB pathway that makes the tumors more sensitive to radiation therapy, which could explain how and why those patients are surviving better.”
Ultimately, this data could be used to identify patients whose therapy can be safely de-intensified in order to treat the tumor, lessen side effects, and enhance quality of life. Now that researchers have more of an understanding of the new mechanism of HPV carcinogenesis, the findings may lead to the development of new, personalized treatments that are more efficient and have fewer side effects.
— Media contact: Kendall Daniels, Communications Specialist, UNC Health | UNC School of Medicine
