Understanding Pancreatic Cancer
If you or a loved one has been diagnosed with pancreatic cancer, you’re likely wondering how to proceed. Where should you seek care? What does treatment involve? Our team of experts at the UNC Lineberger Pancreatic Cancer Center of Excellence is here to guide you in this confusing time and help you make the best decisions for your needs. Below you’ll find some essential information about this complicated disease and learn what we are doing to treat patients with pancreatic cancer at UNC Lineberger.
The Basics
Pancreatic cancer occurs when abnormal cells grow within the pancreas and divide out of control to form a tumor. This form of cancer is difficult to diagnose early, because signs and symptoms are not as obvious as other, more common cancers. The pancreas is located deep inside the abdomen, where tumors are unlikely to be noticed during your routine physical examinations.
Although there are no early warning signs and symptoms can be so vague as not to be noticed, some patients have reported experiencing the following as pancreatic cancer evolves:
- Nausea, vomiting, and unintended weight loss
- Pain in the back and upper abdomen
- Burning sensations in the stomach
- Difficulty digesting fatty foods
- Jaundice (a yellowing of the skin or the whites of the eyes) and/or itchiness
- New onset diabetes
Most cases of pancreatic cancer are only diagnosed after the disease has spread to other parts of the body via the blood and lymphatic systems. At this point, treatment options are more limited. However, improved care methods and early screening and genetic testing for high-risk patients offer some optimism that pancreatic cancer could soon become significantly more treatable.
What does the pancreas do and how does it develop tumors?
The pancreas is an important organ of the digestive system. Within its glandular tissue the pancreas produces enzymes that aid digestion and hormones that help regulate blood sugar levels. The pancreas is made up of two types of tissue, both consisting of cells that can develop tumors:
- Exocrine tissue creates digestive enzymes that are secreted through small channels or ducts to help break down food as it passes through the intestines. Comprises 95% of the pancreas.
- Endocrine tissue creates the hormones insulin and glucagon, which are released into the bloodstream. Comprises the other 5% of the pancreas.
Exocrine and endocrine tumors have different signs and symptoms, are diagnosed with separate tests, and require unique treatments.
The vast majority of patients with pancreatic cancer have pancreatic ductal adenocarcinoma (PDAC), which stems from abnormal exocrine cells and carries tumors that resemble microscopic “ducts.”
The other type, the pancreatic neuroendocrine tumor, develops in islet cells that are responsible for hormone production. These tumors are rarer and tend to be less aggressive and more treatable if discovered early.
Pancreatic Cancer Risk Factors
The factors that put people most at risk of pancreatic cancer are smoking or tobacco use, diabetes, and obesity. Patients who are 55 or older or African American are also at higher risk, as well as those who have family history of pancreatic cancer—two or more first degree relatives (parents, siblings or children) with pancreatic cancer.
How do we test for pancreatic cancer?
Our team of clinicians relies on physical examination, imaging, and tissue biopsies. We conduct a variety of safe tests to find tumors and determine which stage of pancreatic cancer a patient has.

- Blood tests: in addition to monitoring disease progression and tracking treatment effectiveness, some of our tests involve measuring liver function and protein levels in the blood.
- Diagnostic imaging: CT scans, MRI, endoscopic ultrasound, and other methods are used to examine the extent of tumor(s) in the pancreas and figure out whether cancer cells have spread to other parts of the body.
- Biopsy: a small amount of tissue is removed from the pancreas, or a suspected site, and a pathologist inspects this sample under a microscope to assess whether the tumor tissue is benign (noncancerous) or malignant (cancerous). There are multiple types of biopsy including:
- Percutaneous fine-needle aspiration: a needle is inserted through the abdominal wall to extract cells from the pancreas.
- Endoscopic ultrasound: a thin tube called an endoscope is threaded down your throat with a small camera to capture images of the pancreas and a needle that is inserted through the wall of the stomach to collect a pancreatic cell sample.
- Brush or forceps biopsy: similar to the ultrasound, an endoscope with a small brush or forceps attached to the end will be used to gather a sample by brushing the pancreatic/bile duct or snipping cells from these areas.
- Percutaneous fine-needle aspiration: a needle is inserted through the abdominal wall to extract cells from the pancreas.
Based on what we discover through testing, we will then recommend a specific treatment or a combination depending on the stage of a patient’s disease. If testing shows that a tumor is malignant we will use our data to assign a stage of cancer, or the extent to which your tumor has grown or cancer cells have spread.
The Four Stages of Pancreatic Cancer
| I | Tumor is completely contained within the pancreas and less than two centimeters across. |
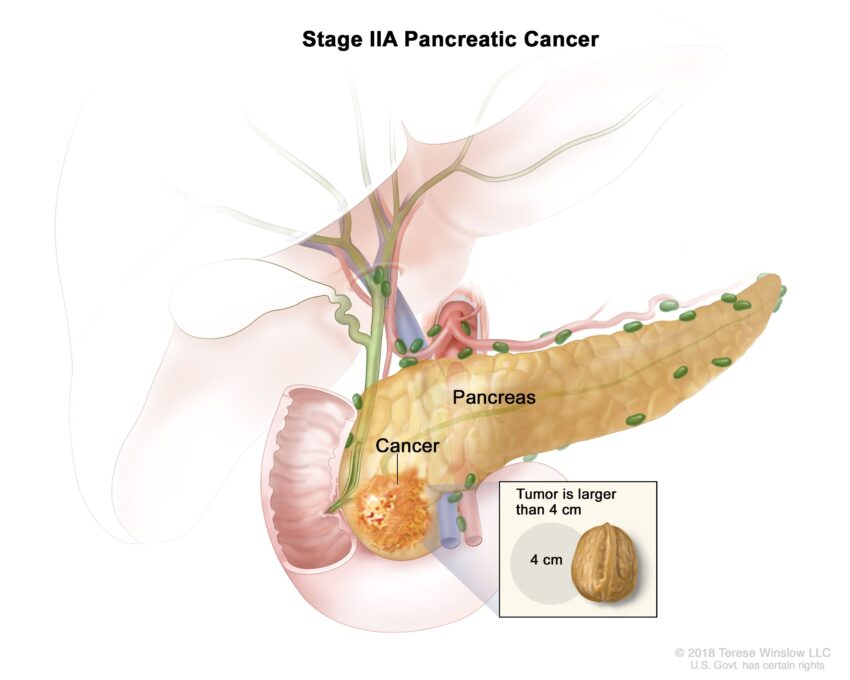
| II | Tumor has begun growing outside the pancreas but not invaded major blood vessels. May have spread to nearby lymph nodes but not farther into the body. |
| III | Tumor is growing outside of the pancreas and moved into nearby large blood vessels or major nerves. |
| IV | Tumor has spread far from the pancreas, such as the liver or inner lining of the abdomen. |
Testing for High-Risk Pancreatic Cancer
Genetic testing and routine screening through diagnostic imaging and/or endoscopic ultrasound can be beneficial to predicting pancreatic cancer and catching tumors while they are still treatable. Patients at greater risk due to family history or various genetic mutations should be screened and genetically tested. The High-Risk Clinic in the UNC Lineberger Pancreatic Cancer Center of Excellence recommends making an appointment for these services if you or someone you know might be at elevated risk.
Pancreatic Cancer Treatment Options and Trials
The most effective methods we currently have for treating pancreatic cancer are surgery, chemotherapy, and radiation. Patient outcomes are significantly better if tumors can be surgically removed, but often tumors have already spread and thus surgery is no longer helpful.
Expert pancreatic surgeons at UNC-Chapel Hill can perform traditional and minimally invasive procedures. If tumors are resectable, or removable via surgery, we will attempt to safely remove them. If they’ve spread and are unresectable with surgery, our radiation and chemotherapy teams will develop the appropriate treatments.
Before surgery or radiation, we might insert a port under the skin of the chest to administer chemotherapy. Ports are basically long-term implanted IVs, used instead of fresh IVs each chemo session to safely shrink tumors and kill cancer cells that spread beyond the pancreas.
After primary treatment, additional chemotherapy might be needed to remove any remaining cancerous cells and reduce the risk of relapse.
Our Research
The world-class researchers, clinicians, and surgeons here at UNC Lineberger constantly collaborate to develop novel targeted therapies and immunotherapy drugs that will hopefully lay the foundation for improved treatment solutions.
Data and outcomes from the clinical setting generate new ideas in the labs, and more recently new insights into the molecular makeup of pancreatic cancer have offered new opportunities to approach this challenging disease. The outstanding research we conduct is pivotal to providing our patients with the best personalized care.
We also encourage patients who might be eligible to join a clinical trial held at our institution. Clinical trials allow us to evaluate promising new drugs and treatment methods that may further improve outcomes for all patients.
Information from clinical trials is invaluable. We recognize the hardship that our patients and families go through and appreciate participants’ commitment to helping all patients with pancreatic cancer experience the best possible care.
Making the right decisions with help
We are optimistic about advancements on the horizon, and we stand with our patients and their loved ones as they navigate diagnosis, treatment and, ideally, recovery. If you would like to request an appointment with our team you can call (984) 974-0000. Please don’t hesitate to reach out to us with any questions or concerns.