Once cancer treatment ends, hopefully with a clean bill of health, most patients hightail it away from the hospital, putting the endless batteries of tests, needle sticks and scans in their rearview mirror. So it’s a rare patient that returns of their own volition, and rarer still, becomes a lab volunteer.

But that’s exactly what David Hesmer did. Hesmer, 28, is a volunteer in the lab of Shawn Hingtgen, PhD, working sometimes weekly or monthly with Hingtgen and Kevin Sheets, PhD, to further the study of glioblastoma, something he knows a lot about.
Hesmer was diagnosed with glioblastoma in 2016, but it wasn’t a straightforward or easy diagnosis. Severe headaches, nausea and abnormal fatigue were passed off as gastritis or a bad hangover, and Hesmer found himself visiting doctors with increased frequency.
“By Labor Day 2017, I was having the worst headache of my life,” Hesmer said. “I began to throw up, and it didn’t stop for days. I couldn’t eat, couldn’t sleep, couldn’t work. Finally, an MRI confirmed that there was a real problem. I had an aggressive brain tumor that needed to come out immediately.”
After being rushed to the N.C. Cancer Hospital, the clinical arm of UNC Lineberger, that same day, Hesmer had surgery and scheduled chemotherapy and radiation treatments. And even though doctors advised against it, Hesmer, naturally, googled his condition.
“I found out what I was dealing with,” he said. “The results are dismal with glioblastoma. It was a pretty big moment for me, understanding what I actually had.”
Making connections
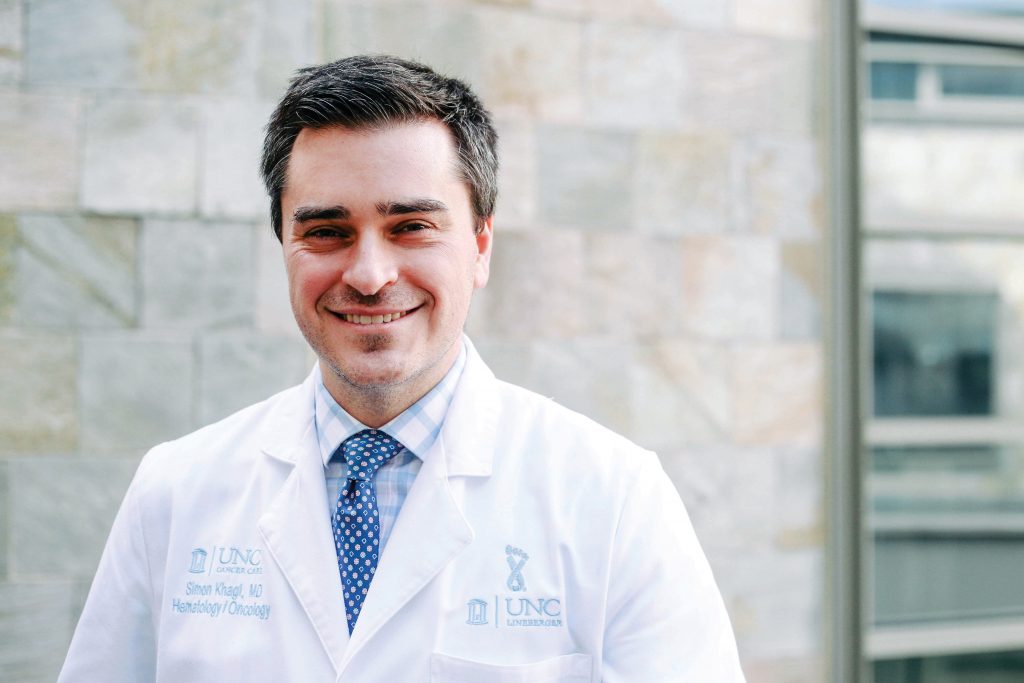
Helping Hesmer cope with the reality of his disease was UNC Lineberger’s Simon Khagi, MD, a neuro-oncologist and chief of UNC Lineberger’s brain tumor program.
“After his initial surgery, a majority of disease was removed. It can’t ever be completely removed, and a rootlike system of cells are left over, so [patients] see a neuro-oncologist,” Khagi said. “I see myself as quarterbacking for my patients; they not only meet me, but they meet the radiation oncology team to discuss that aspect of care.”
Hesmer had an extreme reaction to chemotherapy but worked with Khagi on solutions to the extreme nausea, and while his health wasn’t the greatest, he was able to find something to look forward to while he recovered — a chance to make a difference for other glioblastoma patients in the lab.
Hingtgen’s lab has been exploring using the potential of stem cells to treat terminal cancers, including glioblastoma, and Hesmer learned of the research while still in treatment. “In one random meeting, [Hingtgen] described what they were working on, and it led to me volunteering,” Hesmer said. “They asked me to do it, and I would never have said no to that.”
Seeing research advancements first-hand
Sheets works closely with Hesmer in the lab and said having him volunteer reminds the lab team that their work goes beyond test tubes and pipettes.
“It’s easy to get caught up in the daily grind of the lab; conduct an experiment, crunch the numbers, analyze the data and plan the next experiment,” Sheets said. “Over time, the focus shifts away from the disease and toward the treatment itself. If you’re not careful, you’ll forget the whole reason you’re doing the experiments in the first place – to help people suffering from the disease.”
“We are no longer just trying to shrink his tumor in a mouse,” Hingtgen said. “We are trying to find something that is effective enough and safe enough to potentially treat a friend and fellow lab member. Our science has to be good enough to look David in the eyes and say ‘it works.’ ”
Hesmer said he figured he’d be more like a mascot to the lab team, but they have urged him to participate and have even tried to convince him to do his own study. Hesmer said seeing first-hand some of the research advances into cancers like his is inspiring, and he has full confidence in the skills and insights of the Hingtgen lab team and is hopeful about the research outcomes.
“I’d like to see the stem cell delivery system make it to clinical trials, because I think it will be effective as a therapy,” he said.
While a cure for glioblastoma is not yet a reality, therapies are what keep patients like Hesmer feeling well and optimistic for the future.
“In this position I feel like I’ve been given a purpose, and I wouldn’t have had this opportunity before,” Hesmer said. “To be a part of cancer therapies, even my own, is a very special thing.”
