Researchers at UNC Lineberger Comprehensive Cancer Center have developed a molecule, called uniSTING, that is much more effective than a previously identified molecule, called STING, at activating a biological pathway and spurring a strong anti-cancer immune response in preclinical studies.
The findings appeared in Nature Nanotechnology.
The cGAS-STING biological pathway is known to robustly kickstart the immune system, so it holds great promise to fight cancer. However, drugs that activate this pathway have not produced strong results in clinical trials in fighting many types of cancer. This is due in part to many cancers not expressing the protein(s) that are needed for this pathway or that the pathway is suppressed in the body so the drugs cannot activate the pathway.
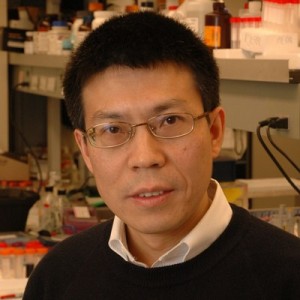
“In my lab and in a collaboration with Dr. Jenny Ting, we bypassed this problem by designing an active STING which we called universal STING, or uniSTING, which does not rely on the expression or activation of native STING,” said UNC Lineberger’s Rihe Liu, PhD, senior co-corresponding author and a professor in UNC Eshelman School of Pharmacy’s Division of Chemical Biology and Medicinal Chemistry.

“The messenger RNA, or mRNA, that encodes uniSTING was delivered to cancer cells by a small fatty nanoparticle delivery system just like the COVID-19 vaccines, and can enter the cells, causing them to activate robust immunity,” Liu said. “We found that uniSTING boosts anti-tumor immunity without activating the pro-tumor pathway, which is a major plus compared to previous attempts using STING drugs.”
The researchers said uniSTING is attractive because it preferentially activates immune stimulating pathways without activating inflammatory pathways which can promote tumor growth.
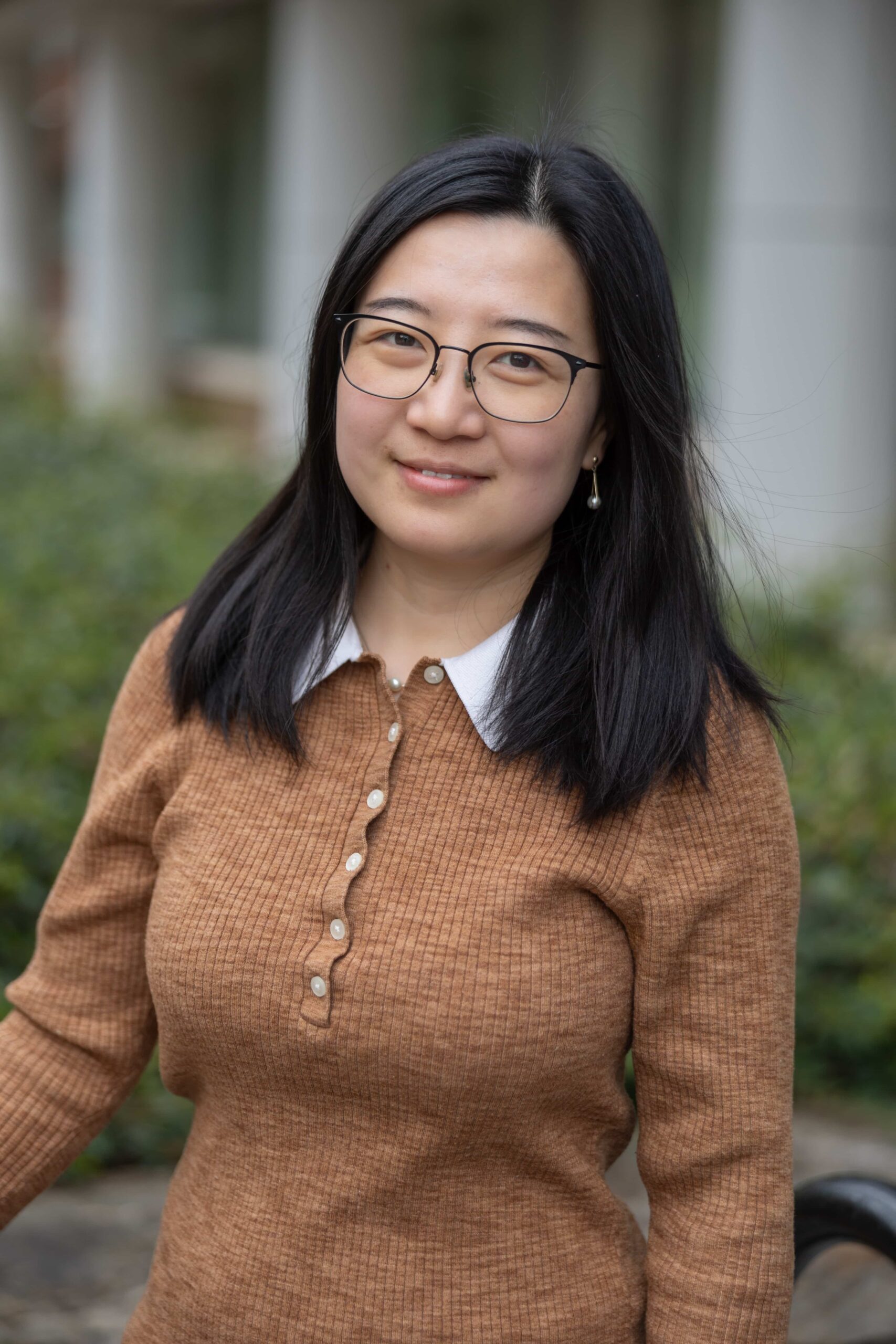
In both human cancer cells and preclinical mouse cancer models, uniSTING overcame a limitation of STING drugs and generated strong antitumor immunity across a variety of advanced cancer types, including mouse models of liver cancer, lung cancer and triple-negative breast cancer, all notoriously difficult-to-treat. This makes it an appealing option for translational applications to humans, particularly for untreatable STING-deficient tumors, noted Jenny Ting, PhD, senior co-corresponding author, the William R. Kenan, Jr., Distinguished Professor of Genetics and director of the Center for Translational Immunology and UNC Lineberger member.
The researchers tested uniSTING in solid tumors to gauge if their methods produced a robust response. Solid tumors are considered more difficult to cure, especially those where anti-cancer drugs can’t infiltrate and activate immune cells very well, have a low number of cell mutations that could be targeted, or exist in microenvironments that suppress tumor activity. The investigators determined that uniSTING was effective, and they speculate it may merit testing in hematopoietic cancer models, such as blood and lymphoid cancers, as well.
“Having now tested uniSTING in cells and in mice, we are hoping that our next step will be to partner with others to move to a clinical development of uniSTING that is much more effective than the STING-related drugs tested so far,” said Sirui Li, PhD, a research associate in Ting’s lab and co-first author of the paper.
Authors and disclosures
In addition to Ting and Liu, the corresponding authors, and Li and Ying Wang, PhD, co-first authors, the other authors are Ellie McCabe, PhD, Lillian Zhang and Andrew M. Withrow, UNC-Chapel Hill; Mengying Hu, PhD, Weill Cornell Medicine, New York; and Yuchen Yang, PhD, Sun Yat-sen University, Guangzhou, China.
The research was supported by grants from Eshelman Innovation (RX03202109 and RX03222104), the University Cancer Research Fund (MCR0634222), and the NIH (R01EB032865, R35-CA232109 and R01-AI029564).
The authors declare no competing interests.
